By Jessie Lei, Neurobiology, Physiology, & Behavior and minor in Human Development, ’24
Author’s Note: Every person and every facet of life was uniquely impacted by the effects of the COVID-19 lockdowns, yet how deep this influence runs can be unclear. Through the eyes of my grandfather, I witnessed first-hand just how detrimental the pandemic was on the progression of his chronic retinal eye disease. In an effort to learn more about current findings on the collateral damage from lockdowns on macular degeneration patients, this review seeks to synthesize relevant research on this growing topic. The hope is that readers come to recognize the real-time irreversible effects that are occurring in patients because of a temporary event and make connections with this information in any way to bring overall awareness.
ABSTRACT
Purpose of Review: Neovascular age-related macular degeneration (nAMD) is an unrelenting disease that leads to complete loss of vision in the global elderly population. Though there have been recent advances in treatment, namely anti-VEGF (vascular endothelial growth factor) injections that slow the progression, its success is contingent on repeated administration. These injections slow the secretion of VEGF by retinal cells to prevent the growth of abnormal blood vessels in the retina. When COVID-19 lockdowns were enforced in 2020, nAMD patients were forced to stop their essential ophthalmic visits. The purpose of this review is to synthesize the results from 5 retrospective studies, which explored the long-term effects nAMD patients were subjected to due to the termination of their eye care during the COVID pandemic.
Main Findings: Severe declines in visual acuity were observed from 2020 to 2021, implying that the visual ability for nAMD patients was declining. This was observed even after treatment visits were resumed after lockdown. An additional set of parameters was used to measure the effects on the structural anatomy of the eye, but results were inconclusive due to contradicting data presented from different studies. For example, the damage inflicted on the macula from abnormal fluid accumulation was reversible after anti-VEGF injections resumed, while in other studies, it was determined that these structural parameters only continued to worsen over time.
Keywords: macular degeneration, neovascular, injections, COVID-19, delay of care
INTRODUCTION
Globally, one of the primary causes of irreversible blindness in older generations is age-related macular degeneration (AMD) [1]. This progressive disease is characterized by a gradual loss of one’s central vision due to the degradation of the macula, an area located in the lining of the back of the eye. It is categorized into two clinical forms, dry and wet, with the latter being responsible for severe central vision loss in 90% of AMD cases [2]. Although the pathogenesis of neovascular, or wet, AMD (nAMD) is still unknown, it is characterized by the proliferation of abnormal blood vessels in the retina. These blood vessels are recruited due to the secretion of the vascular endothelial growth factor (VEGF) by retinal cells. Consequently, the atypical vessels will leak fluid and damage the dense population of color photoreceptors within the macula, causing distorted vision. To track the progression of nAMD, current research supports utilizing best-corrected visual acuity (BCVA) measurements and the analysis of optical coherence tomography (OCT) images [3]. BCVA helps assess the functional health of one’s vision and is measured by having patients read letters of decreasing size from a set distance. OCT scans are best simplified as cross-sectional images of the layers in the retina that help visualize a number of parameters indicative of the eye’s structural integrity.

Treatment Options
Despite nAMD’s prevalence in the aging population, only recently has an effective treatment been developed that helps stabilize vision by preventing damage from blood vessel growth [4]. Prior to this discovery, photodynamic, or light therapy was the main modality of care where light-activated medicine was stimulated by lasers to seal off abnormal blood vessels. But, it had many complications and only focused on reducing the likelihood of further vision loss. Currently, anti-VEGF drugs are the treatment of choice by ophthalmologists because the intravitreal injections into the eye have fewer adverse effects and outperform previous treatments by partially restoring vision [2]. The mechanism of action is through the inhibition of the VEGF pathway expression, which produces the main glycoprotein that causes leaky blood vessels [4]. However, the caveat is that the drug must be continuously administered every few weeks for a variable amount of time (usually 12 weeks) to take effect. This is the only treatment regimen that has seen significant improvements in patients’ control over nAMD progression [5].
COVID-19 and Macular Degeneration
When the COVID-19 pandemic brought global lockdowns in March of 2020, this treatment plan grew difficult to follow because hospitals were placed under strict public health measures. nAMD patients experienced an unplanned discontinuation of injections since virtual ophthalmic visits were unfeasible for this type of care. Adherence to regular treatment visits dropped to as low as 46% during lockdowns [6], and a recent systematic review by Im et al. illustrates how compared to other common retinal eye disorders, nAMD patients were the most susceptible to deterioration of the eye after treatment suspension [7]. Therefore, this literature review seeks to understand how the delay of injection care impacted long-term disease progression after COVID-19 lockdowns in 2020 for patients diagnosed with nAMD that were already receiving treatment.
RESULTS

Decline of Visual Acuity (VA)
As one of the key determinants in nAMD patients’ overall functional capabilities, BCVA is heavily prioritized by researchers. It provides an accurate representation of how sharp their vision is and tracks changes that occur over time. The study conducted by Stattin et al. assessed how VA was compromised in 98 nAMD patients one year after a 9-week treatment deferral due to COVID-19 restrictions [8]. All patients had ophthalmic exams and injections every few weeks after restrictions were lifted where additional data on BCVA changes was collected. By using 95% confidence intervals with p-values of <0.0001 and linear regression models, the analysis revealed a loss of 4.1 ± 8.1 letters in 1 year after lockdown, which was compared against a pre-lockdown average of 2.9 ± 12.7 letters loss in 3 years [8]. Given the context of using small p-values in the analysis, the results yield large ranges but the significant difference in letter loss still illustrates a profound decline in visual acuity. In essence, the typical BCVA decline that would have been observed in nAMD patients over the course of 5 years was witnessed within 1 year due to unintended treatment breaks. Furthermore, because the delay in care expedites the rate of neovascular AMD in patients, anti-VEGF injections offer limited help in slowing that progression down.
Along a similar line, Rego Lorca et al. also demonstrated that 12 months of routine visits were unable to mitigate the immediate VA consequences that stemmed from suspension of treatment in 242 nAMD patients from Spain [9]. Additionally, a statistical model was developed for the sample population to demonstrate what visual loss as part of natural disease progression looked like. This serves as a point of comparison to help identify what percentage of the results could be attributed to injection delay. It was found that an average of 7.2 letters were lost in patients’ BCVA over the duration of COVID-19 lockdowns and the 12 months of resumed follow-up care [9]. Based on the approximated natural rate of vision loss calculation, a 2.5 letter deficit can be credited, thus leaving an average of 4.7 letters lost over the aforementioned time period [9]. This means that capacity wise, nAMD patients experienced a functional decrease in visual clarity by 4.7 letters that can not be explained as part of inevitable nAMD progression. Another way that Rego Lorca et al. presented their findings is that pre-pandemic, 1.6 letters lost/year was expected; but post-pandemic, even with treatments restarted, an average of 3.1 letters lost/year was observed [9]. All of these figures point to a continuing theme that sudden drops in BCVA scores is the direct product of treatment discontinuation from the pandemic. Sevik et al. further supported this pattern in a paper that directly compared the outcomes of two different groups – those that delayed their appointments by an average of 3 months during the pandemic (group 1) and those that remained consistent (group 2) [10]. Each group consisted of 30 to 50 nAMD patients from Istanbul and were evaluated periodically for 6 months after lockdowns. It was discovered that with normal injections and follow-up post-lockdown, BCVA remained stable in group 1 while group 2 continued to suffer from statistically significant decreases that were not regained within 6 months [10]. With other possible confounding variables accounted for during the inclusion and exclusion of patient selection in this retrospective study, the only variable that can be attributed for the difference in functional outcomes is the postponement in treatment care.
Variable Impacts on Structural Eye Health
In contrast to the prior parametric analysis, there is not one single measurement that can appropriately represent the complexities of the eye as a whole and determine its structural health. Instead, the majority of researchers will examine a variety of anatomical characteristics that can be seen on OCT images. For Kim et al., they chose to study the maximum subretinal fluid (SRF) height, which conveys how much abnormal fluid has accumulated under the retina, as the main indicator of disease activity in 57 Korean nAMD patients [11]. They found that SRF height initially improved but by the 6-month check-up, had significantly worsened compared to baseline. At the end of the study, SRF height increased by 37 μm, which was about 18.9% higher than the recorded baseline value prior to COVID-19 lockdowns [11]. Because of the unique methodology employed where follow-ups occurred in 2-month intervals, researchers were able to catch nuanced fluctuations in progress results, like the temporary morphological improvements in SRF height following the return to treatment regimen. But that quickly deteriorated by the 6-month mark, emphasizing the rapid and unpredictable effects that delayed injections could have on disease activity.
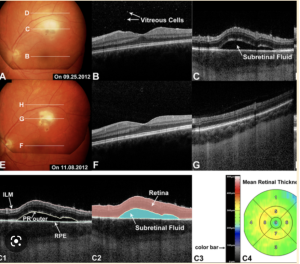

Interestingly, the article by Rego Lorca et al. completely contradicts previous conclusions from Kim et al. [11] by exhibiting that their sample population was able to anatomically recover to pre-pandemic state with 12 months of continuous treatment [9]. Active disease was defined as showing evidence of SRF and macular neovascularization (MNV), which is the proliferation of atypical blood vessels on the retina, on OCT images. Prior to the lockdown, SRF was present in 25.7% of the sample population, which increased to 28.2% during lockdowns, and decreased to 14.7% after 12 months of routine check-ups. Similarly, the percentage of MNV within nAMD participants before lockdown was 65.3%, increased to 79.6% during lockdowns, and decreased to 51% after [9]. Thus, the structural deterioration of the eye was demonstrated to be fully reversed and improved across two separate parameters in this specific paper.
Rozon et al. brings in a plausible explanation for the previous discrepancies in their research which assesses the influence that delayed follow-ups had on 351 nAMD patients in Canada [12]. SRF and central foveal thickness (CFT) parameters on OCT images were used to define the structural integrity of the eye. CFT refers to how far off the thickness of the retinal center is from the normal range, because the thicker it is, the higher the likelihood of unwanted fluid accumulation within the retina. After 6 months of rigorous injections, the delay in follow-ups was linked to significant worsening of SRF parameters, while CFT measurements were normalized within the same time frame. SRF increased from 12.4% to 19.1% by 6 months; CFT levels began at 256.1 μm and fluctuated throughout the 6 months, but eventually ended up at 255.7 μm [12]. This provides further clarification on anatomical impacts because multiple different characteristics on OCT images were considered. It illustrated how some features may
improve over the 6-month period while others remain at a deficit, therefore depending on the parameter chosen by researchers, it will yield different data.
DISCUSSION
Analysis of Findings
Amongst these reviewed articles, the combination of statistics highlight the persistent decline in visual loss that appears to be irreversible since pre-pandemic functional capabilities were not recovered in any nAMD patients [8-10]. Even after undergoing intense care following the interruption of visits, visual acuity continues to decline at alarming rates that current treatments cannot seem to dampen. On the other hand, no definite structural outcome could be confidently concluded because the data of each paper do not fully corroborate with one another [9, 11-12]. Some depict the possibility of restoring any anatomical damage sustained during the delay [10], while others express the worsening of structural parameters in the long-term [11-12]. Therefore, it is evident that additional research which explores a multitude of OCT features is needed before a conclusion on the reversibility of damage on the structural integrity of the eye can be made. However, a contradicting paradigm starts to form as there is a high possibility that the functional and structural impacts are complete opposites, which may imply a more complex issue.
Strengths and Limitations
Limitations of this review and its sources may help explain why this contradicting paradigm emerged from the findings. One of the biggest weaknesses is that the majority of the studies employed similar experimental designs that were retrospective in nature. Since it would be unethical to create a scenario in which treatment is purposefully delayed, this limitation is inevitable but should still be addressed because retrospective papers tend to supply a degree of selective bias during patient selection. Furthermore, in the article by Rozon et al., additional focus on risk factors and minimal acknowledgement of the COVID-19 pandemic’s contribution to the delayed follow-ups act as notable limitations to the relevancy of this source [12]. However, it still provided invaluable insight into why inconsistencies associated with using OCT measurements as a dependent variable occur that other researchers did not identify. Despite these disadvantages, there are still many notable strengths that this review has to offer. Researchers were able to eliminate possible confounding variables and establish a cause-effect relationship by including control groups [10], and statistical models of natural nAMD history [8-9]. Additionally, there is a wide diversity of patients from different countries represented, ensuring that the results of this review can be extrapolated and applied to nAMD patients on a global scale.
Application of Findings
As for implications, it is clear that nAMD injection treatments should be given priority in the event of another lockdown because consistency is necessary for positive effects. Patients and health professionals should maintain strict care regimens to ensure that further regression is not seen. It is recommended that research still be conducted in this topic, especially because there is potential to examine what effects from this lockdown period remain 5 or 10 years into the future and provide more evidence on anatomical impacts.
CONCLUSION
When thoroughly considering all five core sources, there is a distinguishable response to the primary research question about the long-term deleterious effects on functional and structural eye health that were felt by nAMD patients after COVID-19 lockdowns caused unexpected gaps in treatment. Specific themes about the profound negative impacts had on visual acuity and the uncertainty regarding ramifications on the morphological health of the eye were uncovered. To limit the collateral effect of this pandemic on patients’ ophthalmic health, healthcare providers should proactively check in on nAMD patients. They should also place emphasis on performing additional research to better understand the long-term effects of lockdowns and if morphological damage sustained in the eye can be fully restored.
The author declares no conflict of interest.
REFERENCES (FULL)
- Learn about age-related macular degeneration. Centers for Disease Control and Prevention. Published November 23, 2020. Accessed March 14, 2023. https://www.cdc.gov/visionhealth/resources/features/macular-degeneration.html
- Flores R, Carneiro Â, Vieira M, Tenreiro S, Seabra MC. Age-Related Macular Degeneration: Pathophysiology, Management, and Future Perspectives. Ophthalmologica. 2021;244(6):495-511. doi:10.1159/000517520
- Ho AC, Albini TA, Brown DM, Boyer DS, Regillo CD, Heier JS. The Potential Importance of Detection of Neovascular Age-Related Macular Degeneration When Visual Acuity Is Relatively Good. JAMA Ophthalmol. 2017;135(3):268–273. doi:10.1001/jamaophthalmol.2016.5314
- Song D, Liu P, Shang K, Ma YB. Application and mechanism of anti-VEGF drugs in age-related macular degeneration. Front Bioeng Biotechnol. 2022;10. doi:10.3389/fbioe.2022.943915
- Augsburger M, Sarra G-M, Imesch P. Treat and extend versus pro re nata regimens of ranibizumab and aflibercept in neovascular age-related macular degeneration: A comparative study. Graefes Arch ClinExp Ophthalmol. 2019;257(9):1889-1895. doi:10.1007/s00417-019-04404-0
- Rothaus K, Kintzinger K, Heimes-Bussmann B, Faatz H, Lommatzsch AP. Impact of the COVID 19 Pandemic on Treatment of nAMD via a Portal-Based Collaboration. Klin Monbl Augenheilkd. 2022;10.1055/a-1806-2474. doi:10.1055/a-1806-2474
- Im JHB, Jin Y-P, Chow R, Dharia RS, Yan P. Delayed anti-VEGF injections during the COVID-19 pandemic and changes in visual acuity in patients with three common retinal diseases: A systematic review and meta-analysis. Surv Ophthalmol. 2022;67(6):1593-1602. doi:10.1016/j.survophthal.2022.08.002
- Stattin, M., Ahmed, D., Graf, A. et al. The Effect of Treatment Discontinuation During the COVID-19 Pandemic on Visual Acuity in Exudative Neovascular Age-Related Macular Degeneration: 1-Year Results. Ophthalmol Ther. 2021;10, 935–945. doi:10.1007/s40123-021-00381-y
- Rego-Lorca D, Valverde-Megías A, Fernández-Vigo JI, et al. Long-term consequences of covid-19 lockdown in neovascular AMD patients in Spain: Structural and functional outcomes after 1 year of standard follow-up and treatment. J Clin Med. 2022;11(17):5063. doi:10.3390/jcm11175063
- Sevik, M.O., Aykut, A., Özkan, G. et al. The effect of COVID-19 pandemic restrictions on neovascular AMD patients treated with treat-and-extend protocol. Int Ophthalmol. 2021;41, 2951–296. doi:10.1007/s10792-021-01854-6
- Kim J-G, Kim YC, Kang KT. Impact of delayed intravitreal anti-vascular endothelial growth factor (VEGF) therapy due to the coronavirus disease pandemic on the prognosis of patients with neovascular age-related macular degeneration. J Clin Med. 2022;11(9):2321. doi:10.3390/jcm1109232
- Rozon J, Hébert M, Laverdière C, et al.. Delayed Follow-Up in Patients with Neovascular Age-Related Macular Degeneration Treated Under Universal Health Coverage. Retina. 2022; 42 (9): 1693-1701. doi:10.1097/IAE.0000000000003512