By Shubhang Bhatt, Neurobiology, Physiology, and Behavior, ’15
Author’s Note:
“What is Myasthenia Gravis?” aims at informing the readers about the mechanism of action, symptoms, diagnosis, and treatment of Myasthenia Gravis. Fatigue and muscle weakness is something that today’s working population has learned to ignore, and this has prevented MG from early detection. Proper treatment is necessary for this potentially life-threatening condition. I decided to write about this topic after reading a case study for one of my internships. I hope the readers will look out for signs like the drooping of eyelids, muscle weakness, and difficulty in swallowing for the early detection of this rare autoimmune disease.”
Myasthenia gravis (MG), “grave muscle weakness” in Greek, is a rare autoimmune neuromuscular disease in which the body’s defense mechanism goes awry and attacks its own cells. According to the National Institute of Neurological Disorders and Stroke, patients with MG complain of varying degrees of worsening muscle weakness in different parts of the body, such as in one or both eyes, face, or limbs. If the condition affects respiratory muscles, it can cause airway obstruction, which can lead to a life-threatening situation called myasthenia crisis (2015). Understanding MG’s mechanism of action, symptoms, and diagnosis can vastly improve the prognosis of this disease.
Usually, our immune system protects us from foreign elements that enter our bodies by creating “soldiers” called antibodies to destroy these elements. During human development, these antibodies undergo a kind of orientation wherein they are trained to recognize self from nonself proteins. A selection process at the end of this session eliminates the antibodies that react strongly with self proteins (Berg 2002). However, in rare cases such as MG, the immune system fails to successfully undergo this process and produces antibodies against its own cells, causing autoimmunity (NLM 2015).
Picture Courtesy of MA
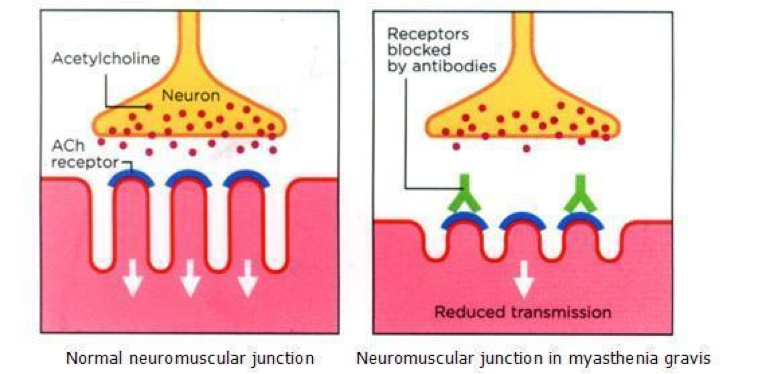
The autoimmunity in MG affects the receptors in the neuromuscular junction (NMJ), or the space between nervous cells and the muscles they control. As the nerve impulse travels down a normal neuronal cell, it communicates by releasing acetylcholine (ACh), a chemical messenger called a neurotransmitter, into the NMJ. ACh then binds to complementary receptors called acetylcholine receptors (AChR) on the adjoining cell. Upon the binding of these chemicals at the receptors, a desired effect is produced, which can lead to further propagation of the impulse to another neuron and eventually cause muscular movement. In MG, the body’s defense system, which usually produces antibodies against foreign elements, makes antibodies against its own cells that bind to cell-specific receptors. This prevents the binding of ACh to the receptors as shown in the figure and leads to their further internalization and subsequent degradation. Consequently, the message is not passed from the cell, resulting in either weakened or no muscle contraction (NINDS 2015). It is, therefore, of prime importance to detect the symptoms resulting from the reduced availability of these receptors at the NMJ for a better prognosis.
MG can be difficult to diagnose definitively, as its initial symptoms are similar to other plausible autoimmune diseases. Therefore, the patient’s symptoms should be analyzed for an accurate MG diagnosis as, in most cases, the onset of the disorder is sudden and is not always a tell-tale myasthenia gravis case. MG is characterized by the decay in muscle strength after use and improvement upon rest. The first noticeable symptoms include the drooping of eyelids (ptosis) and double vision (diplopia). Generalized myasthenia, or weakness all over the body, develops in patients within three years if they initially experience trouble with ocular (eye) muscles (Rubin 2014). Additional symptoms include an unstable gait, a change in facial expression, difficulty chewing and swallowing, shortness of breath, and weakness in the limbs, fingers, and neck. While the symptoms are usually well managed and patients can live comfortably, early detection is key because it can prevent the condition from exacerbating (NINDS 2015).
One of the preliminary ways to diagnose MG is to check for disruption in eye movements or muscle strength. These changes in eye movement and muscle strength can occur without altering the patient’s sensitivity to touch. This occurs because MG is an isolated neuromuscular disease, a disease that does not affect any other system like the sensory system. A more quantifiable way of diagnosing is performing a special blood test to detect AChR antibodies in the blood sample. This test is of high validity, as 80-90% of patients with generalized myasthenia gravis test positive (Rubin 2014). Moreover, the specificity of this test significantly decreases in the absence of ocular symptoms. In another test called electromyography, a repetitive electrical impulse is given to the affected muscle. In 60% of the patients with myasthenia gravis, the muscle response will dissipate over time; that is, the patients’ response to the electrical stimulus will lessen progressively (Rubin 2014). Occasionally, another test is performed during which a drug called edrophonium is administered. If a patient is positive for MG, edrophonium relieves activity-induced muscle fatigue. Nonetheless, this result can be seen in patients with other neurological conditions as well, or if performed in patients without droopy eyelids. A follow-up CT or MRI scan should be performed to check for thymus enlargement, a condition called thymic hyperplasia, prevalent in 65% of MG patients (Rubin 2014). While doctors can utilize various tests to diagnose MG, these tests may provide non-specific results, and thus, more than one test should be performed to confirm the diagnosis.
It is estimated that only 1 in 5,000 Americans are affected by MG, but the actual number may be higher due to the fact that many individuals may be undiagnosed until they reach advanced stages (Juel and Massey 2007). Even though the disease can occur at any age and to anyone, it is more common among women under 40 and men above 60 years of age (NINDS 2015). It is, therefore, essential to have an unambiguous early diagnosis in order to follow-up with proper treatment, as the condition may eventually affect the respiratory muscles, causing airway obstruction.
While there is no known medication for treating the autoimmunity caused by the immune system attacking the ACh receptors, drugs that help manage symptoms are typically prescribed. A class of drugs called anticholinestrase helps relieve symptoms by increasing the duration and availability of ACh in the NMJ and preventing its enzymatic breakdown by acetylcholinestrase. Additionally, steroids are prescribed to suppress the patient’s immune system, reducing the production of antibodies that might target patients’ own cells. However, when taking steroids, caution has to be taken because the patient becomes more vulnerable to other garden variety diseases like the common cold and strep throat, which are otherwise preventable by an intact immune system. Finally, a procedure called thymectomy, or the surgical removal of the thymus gland, can be performed, and it has shown both permanent and temporary improvement in 80% of the cases of MG (Rubin 2014).
Even though MG is a potentially fatal autoimmune disease, it is not as “grave” as it used to be. The latest technological advancements in diagnoses and treatments has made the term “gravis” redundant or unnecessary in MG, with patients having a normal life expectancy after appropriate care (NINDS 2015). Since the symptoms are similar to many other neurological disorders like muscular sclerosis and muscular dystrophy, emphasis should be given to early and accurate diagnosis for effective disease remission. In my opinion, individuals should undergo at least two tests to accurately confirm MG and avoid a false positive. An AChR antibody test could be used, since it is an indicator of an autoimmune disease, and an electromyography test could be administered, since it indicates a neuromuscular disorder. This condition is a good example of how our defense systems can malfunction and cause serious damage to the functioning of our bodies.
Work Cited
Berg JM, Tymoczko JL, Stryer L. 2002. Immune Responses Against Self-Antigens Are Suppressed. [Internet]. Biochemistry. New York: W H Freeman; [cited 2016 Jan 5] 5(33.6). Available from: http://www.ncbi.nlm.nih.gov/books/NBK22378/
Juel, V. C., & Massey, J. M. 2007. Myasthenia gravis. Orphanet Journal of Rare Diseases; [cited 2015 Oct 8]; 2, 44. Available from: http://www.ojrd.com/content/2/1/44http:///h
[MA] Understanding Myasthenia Gravis. c2010. [Internet]. Myasthenia.Asia; [cited 2015 Oct 8]. Available from: http://www.myasthenia.asia/news.aspx?category=1http:///h
[NINDS] National Institute of Neurological Disorders and Stroke. 2015. Office of Communications and Public Liaison. National Institute of Health. Myasthenia Gravis Fact Sheet [Internet]; [cited 2015 Oct 8]. Available from: http://www.ninds.nih.gov/disorders/myasthenia_gravis/detail_myasthenia_gravis.htmhttp:///h
[NLM] National Library of Medicine. 2015. Autoimmune Diseases; [cited 2015 Oct 8]. Available from: https://www.nlm.nih.gov/medlineplus/autoimmunediseases.htmlhttp:///h
Renton AE, Pliner HA, Provenzano C, et al. 2015. A Genome-Wide Association Study of Myasthenia Gravis. JAMA Neurol. [Internet]. [cited 2015 Oct 8] 72(4): 396-404. Available from: http://archneur.jamanetwork.com/article.aspx?articleid=2091915http:///h
Rubin M. 2014. Myasthenia Gravis [Internet]. Merck Manual; [cited 2015 Oct 8]. Available from: http://www.merckmanuals.com/professional/neurologic-disorders/peripheral-nervous-system-and-motor-unit-disorders/myasthenia-gravishttp:///h